Pediatric tachycardia algorithm
 Written by
Jessica Munoz DPN, RN, CEN
Written by
Jessica Munoz DPN, RN, CEN
Changes: Copy edit and tachycardia protocol review
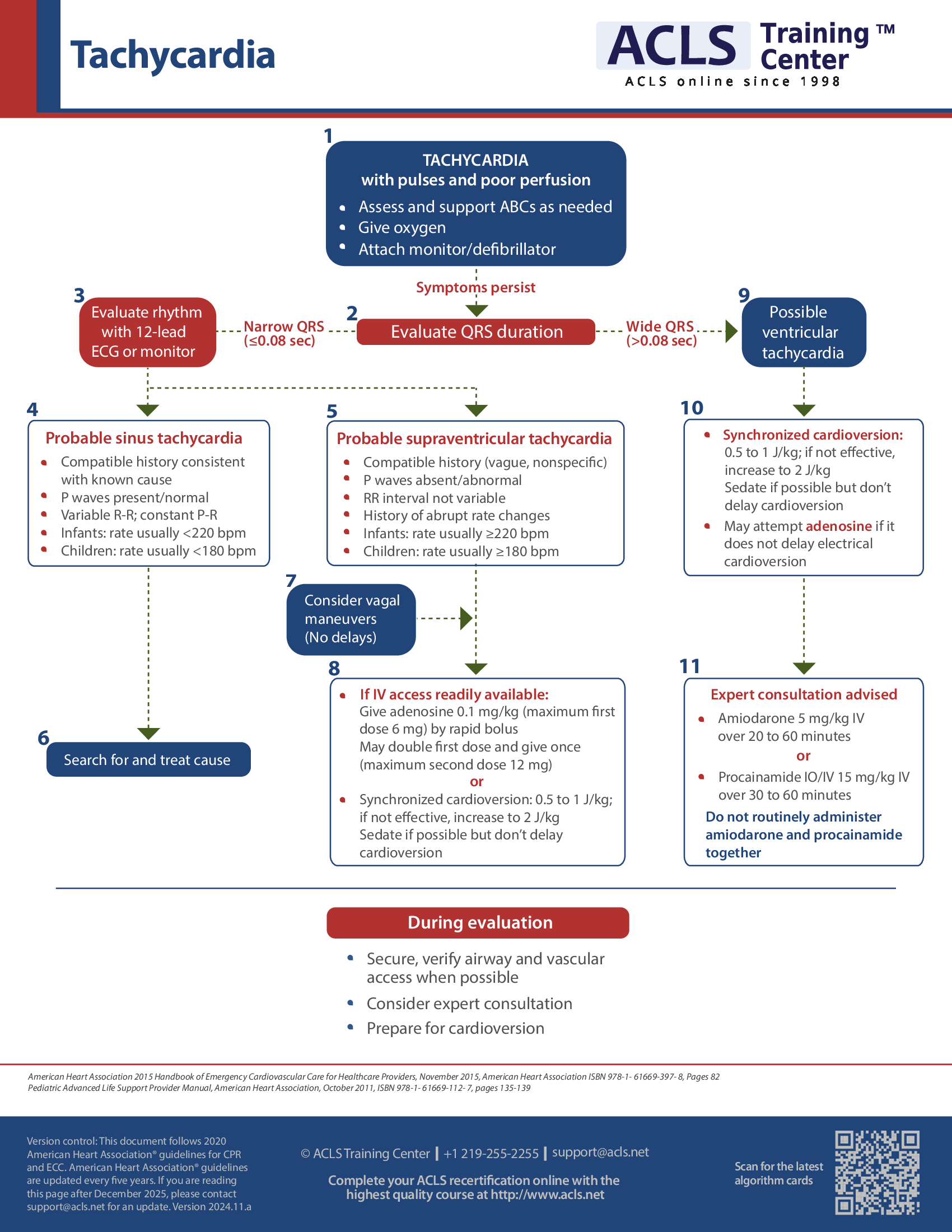
When a child presents with tachycardia with pulses but poor perfusion, assess and support ABCs as needed, give oxygen, and attach the monitor/defibrillator as soon as possible.
Printed crash cart cards

Order the full set of printed crash cart cards.
Pediatric tachycardia with a pulse and poor perfusion algorithm
The approach of evaluation and care for tachycardic children with pulse but poor perfusion is as follows.
The first step is identification of the underlying cause and its subsequent treatment. Quickly, a patent airway should be maintained with assisted breathing or with oxygen.
Heart rhythm should be identified along with monitoring blood pressure and oximetry. There should be access to IV/IO. If available, proceed with a 12-lead ECG without delaying therapy.
Next, the QRS duration needs to be assessed. If the duration is narrow (≤ 0.09 sec), then proceed with a 12-lead ECG or monitor the heart rhythm.
Sinus tachycardia is suspected if: consistent with known cause; there is compatible history, constant PR but variable R-R, and P waves are normal or present. For children, the rate is usually greater than 180/min and for infants the rate is generally greater than 220/min. If sinus tachycardia is present, the cause needs to be found and then treatment initiated.
Supraventricular tachycardia is suspected if: there is a history of abrupt rate changes or compatible history (nonspecific, vague); non-variable HR; P waves are absent or abnormal; for children the rate is usually ≥ 180/min and for infants, the rate is generally ≥ 220/min. If it is supraventricular tachycardia, vagal maneuvers should be considered without delay. Adenosine should be administered in presence of access to IV/IO. However, if adenosine is found to be ineffective or there is no IV/IO access, synchronized cardioversion should be considered.
If the QRS duration is wide (> 0.09 sec), ventricular tachycardia is suspected, which may be caused by cardiopulmonary compromise. If that is the reason, then there will be symptoms of shock, hypotension, and acutely changed mental status. In such a case, synchronized cardioversion should be considered. However, if the QRS is monomorphic and the heart rhythm is regular, adenosine may be considered.
Subsequently, one should consult an expert and consider amiodarone or procainamide.
Details of the dosage to be administered:
For synchronized cardioversion (low energy shock): one may initiate with 0.5–1.0 J/kg and increase up to 2 J/kg if the initial dose is found ineffective. Sedation may be provided but without any delays in cardioversion.
For adenosine IV/IO dosage: initiate with a rapid bolus dose of 0.1 mg/kg and increase up to a maximum of 6 mg/kg. This should be followed by a second bolus dose of 0.2 mg/kg and increased up to a maximum of 12 mg/kg.
Procainamide IV/IO dosage: over a duration of 30–60 min, administer 15 mg/kg.
Amiodarone IV/IO dosage: over a duration of 20–60 min, administer 5 mg/kg. However, procainamide and amiodarone should not be routinely administered together.

Planning to certify/recertify ACLS?
Get a reminder when you need to take the exam
Please verify or enter a different email address:
How we reviewed this article
Our experts continually monitor the medical science space, and we update our articles when new information becomes available.
-
Current versionMail the author of this pageEmail
- Jun 27, 2023
-
Copy edited by:
Copy editorsChanges: Copy edit and tachycardia protocol review - Jul 29, 2021
-
Written by: