Pediatric bradycardia algorithm
 Written by
Jessica Munoz DPN, RN, CEN
Written by
Jessica Munoz DPN, RN, CEN
Changes: Copy edit and protocol review
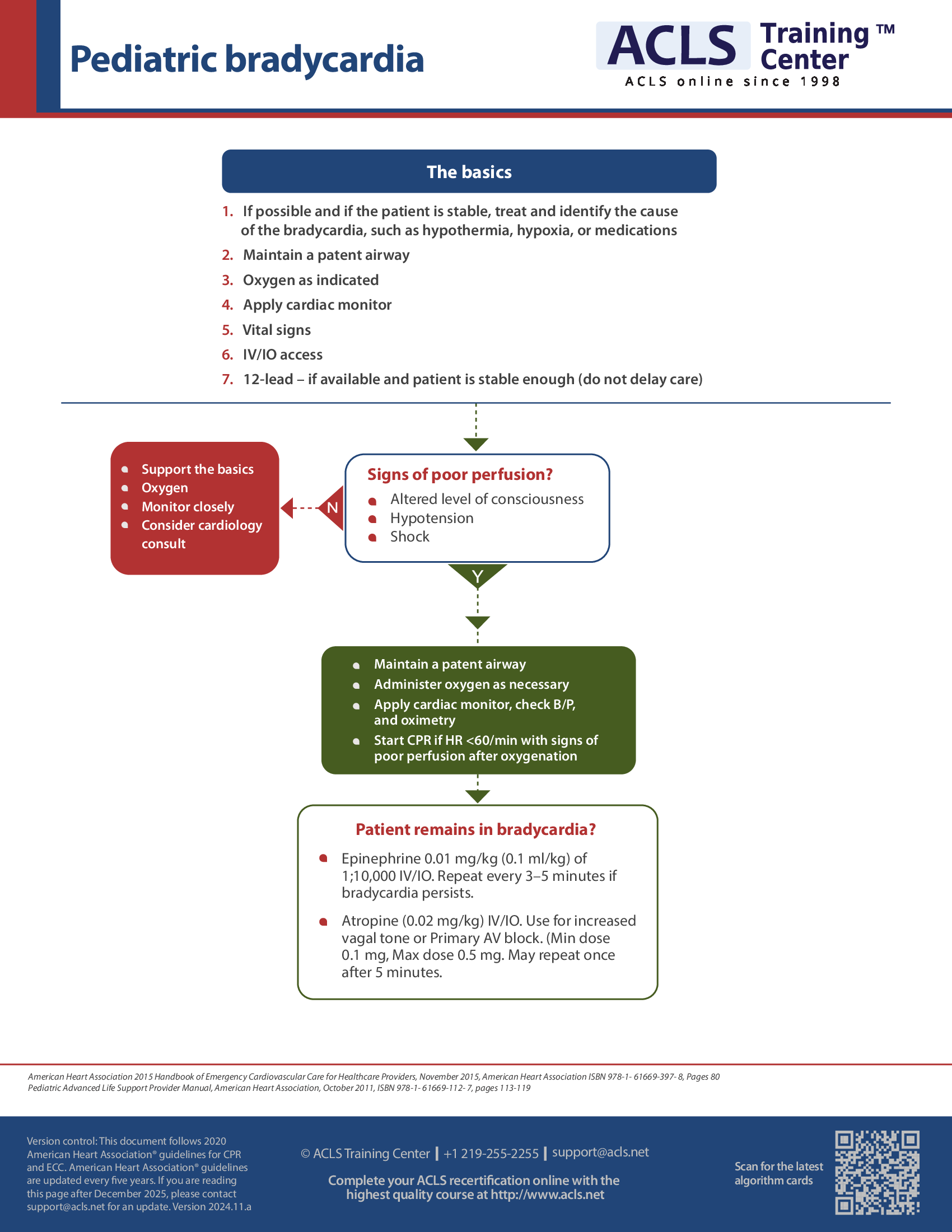
A pediatric patient with symptomatic bradycardia needs the possible causes identified and treated such as hypothermia, hypoxia, or medications. Always maintain a patent airway and apply oxygen for saturation of less than 94% or signs of respiratory distress. Place the patient on a cardiac monitor and monitor vital signs. Obtain IV access or IO if the patient is unstable and IV access is unattainable. Continue to monitor the patient and consider a cardiology consult.
If the patient is unstable and showing signs of poor perfusion such as altered level of consciousness, hypotension, or signs of shock, immediate treatment is required. Maintain a patent airway and apply oxygen as necessary. Place the patient on a cardiac monitor and check B/P and oximetry. If the patient continues to show signs of poor perfusion after oxygenation therapy and the heart rate decreases under 60 beats per minute, start CPR. If the patient remains bradycardic administer epinephrine 0.01 mg/kg IV/IO. This may be repeated every 3–5 minutes for bradycardia. Atropine 0.02 mg/kg IV/IO can be given if the patient has an increased vagal tone if they have 2nd or 3rd degree AV block.
Pediatric bradycardia with a pulse and poor perfusion algorithm
This algorithm outlines the evaluation and care for bradycardia in children with the presence of a pulse and poor perfusion.
In such cases, the first step should be the identification of the underlying cause and its subsequent treatment. A patent airway should be maintained along with assisted breathing or oxygen as necessary. Heart rhythm should be identified along with monitoring blood pressure and oximetry. If available, proceed with a 12-lead ECG without delaying therapy. IV/IO access is required.
If the child is no longer in a state of cardiopulmonary compromise (as indicated by symptoms of shock, hypotension, or acutely altered mental status), then the child may be put under supportive observation and provided with oxygen while awaiting consultation with an expert healthcare provider.
However, if the cardiopulmonary compromise continues with a heart rate less than 60/min, despite adequate ventilation and oxygenation, then CPR should be administered. Even after CPR, if the bradycardia persists, epinephrine or atropine (for primary AV block or increased vagal tone) may be administered.
The basic idea should be to treat the underlying cause along with the consideration of transvenous pacing/transthoracic pacing. If bradycardia does not persist, then the patient should be put under observation and supported with ABCs while awaiting consultation with an expert healthcare provider.
Cardiac arrest algorithm may be followed if pulseless arrest develops.
Details of the dosage:
Atropine IV/IO dosage: 0.02 mg/kg may be administered, which may be repeated once more. The minimum dose is 0.1 mg while the maximum dose is 0.5 mg.
Epinephrine IO/IV dosage: 0.01 mg/kg (0.1 mL/kg of 1:10000 concentration) may be administered; repeated after each 3–5 minutes. ET dose may be given (0.1 mg/kg) if IV/IO access is unavailable and endotracheal tube is in place.
Printed crash cart cards

Order the full set of printed crash cart cards.

Planning to certify/recertify ACLS?
Get a reminder when you need to take the exam
Please verify or enter a different email address:
How we reviewed this article
Our experts continually monitor the medical science space, and we update our articles when new information becomes available.
-
Current versionMail the author of this pageEmail
- Jun 27, 2023
-
Copy edited by:
Copy editorsChanges: Copy edit and protocol review - Jul 29, 2021
-
Written by: