Pediatric cardiac arrest algorithm—advanced
 Written by
Jessica Munoz DPN, RN, CEN
Written by
Jessica Munoz DPN, RN, CEN
Changes: Corrected compression parameters and medication dosing per AHA PALS
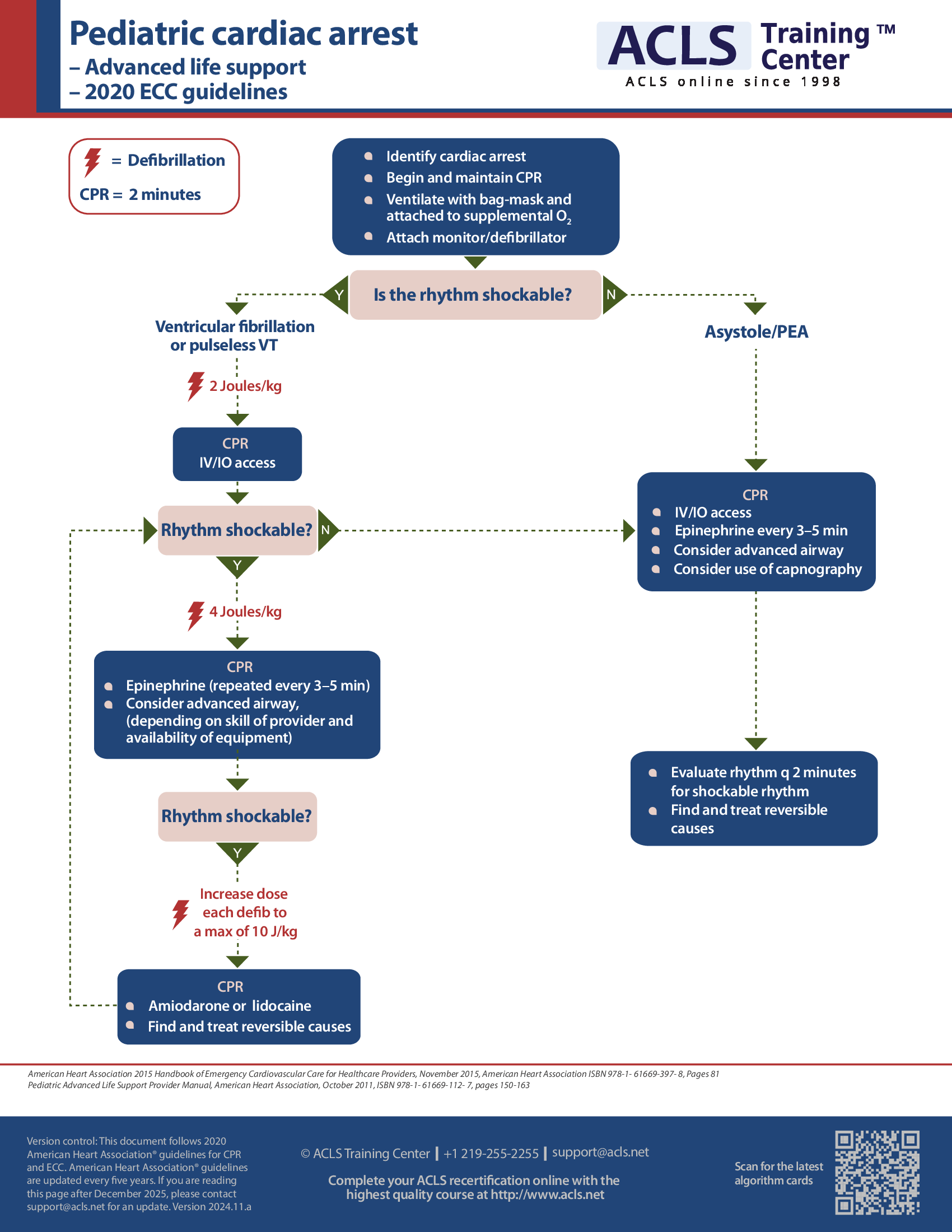
Pediatric cardiac arrest algorithm
The pediatric cardiac arrest algorithm outlines the steps of care and management of infants with cardiac arrest.
Upon finding a child in cardiac arrest, one should shout for help and immediately activate the emergency response team. Meanwhile, initiate CPR, attach AED leads, and provide oxygen. If the rhythm is ventricular fibrillation (VF)/ventricular tachycardia (VT) then provide shock followed by CPR for 2 min along with IO/IV access. At this stage, a second shock may be given followed by another round of CPR for 2 min along with the administration of epinephrine every 3–5 min. Advanced airway may also be considered. Again, if the rhythm is shockable, another shock may be given followed by CPR for 2 min along with amiodarone administration.
However, if the rhythm is asystole or pulseless electrical activity (PEA) then no shock should be given. Instead, CPR should be administered for 2 min along with the provision of IO/IV. Epinephrine may be given every 3–5 min and advanced airway may be considered. If after this stage, the rhythm becomes shockable, shock is administered, followed by CPR. If the same rhythm persists, continue CPR for 2 min.
The assessment should be made based on the rhythm detected. If the AED shows an organized rhythm, pulse should be checked. If the pulse is present, post-cardiac arrest care should be given.
#7: Details and doses of the pediatric cardiac arrest algorithm
#7: Details and doses of the pediatric cardiac arrest algorithm
Quality of CPR: Compress at least 1/3 of the anterior-posterior chest diameter to allow a complete recoil of the chest. Interruptions between compressions should be minimized as much as possible, while avoiding excessive ventilation. In every 2 minute interval, compressor may be rotated. In absence of any airway, the compression-ventilation ratio is 15:2, while in presence of advanced airway, continuous chest compressions and 8–10 breaths per minute should be maintained.
Defibrillation (unsynchronized cardioversion—high energy shock): the first shock is of 2 J/kg followed by 4 J/kg (second shock). Subsequent shocks should be greater than 4 J/kg but not more than 10 J/kg.
Drug therapy: epinephrine IO/IV dosage: 0.01 mg/kg (0.1 mL/kg of 1:10000 concentration) may be administered; repeated after each 3–5 minutes. ET dose may be given (0.1 mg/kg) if IO/IV access is unavailable and endotracheal tube is in place.
Amiodarone IO/IV dosage: during cardiac arrest, 5 mg/kg bolus is given, which may be repeated for pulseless VT or refractory VT up to 2 times.
Provisions of advanced airway: supraglottic advanced airway or endotracheal airway may be warranted. A capnometry or waveform capnography may be used for confirming and monitoring the placement of endotracheal tube. One breath every 6–8 seconds should be given once the advanced airway is in place (i.e., 8–10 breaths per minute).
Provisions of ROSC (return of spontaneous circulation): pulse and blood pressure are present. Intra-arterial monitoring shows the presence of spontaneous arterial pressure waves.
Reversible causes include: acidosis (hydrogen ion), hypoxia, hypovolemia, hypothermia, hypo/hyperkalemia, hypoglycemia, toxins, cardiac tamponade, pneumothorax tension, coronary thrombosis, and pulmonary thrombosis.
#3: Pediatric septic shock algorithm
#3: Pediatric septic shock algorithm
This algorithm outlines the steps required for the care of children with septic shock.
Assess the child and recognize any change in the mental status or perfusion, blood flow through the circulatory system. The child should be provided with adequate ventilation and oxygen while establishing vascular access. Resuscitation should be immediately initiated as per the guidelines of PALS.
Ionized calcium, lactate, glucose, arterial blood gasses (ABG) or venous blood gasses (VBG), complete blood count (CBC), and cultures may also be considered.
In the first hour of septic shock, repeated isotonic crystalloid boluses are administered at 20 mL/kg to the child. If no respiratory distress, rales (small clicking, bubbling, or rattling sounds in the lungs), or hepatomegaly (enlarged liver); 4 or more boluses may be given.
Hypocalcemia and hypoglycemia need to be corrected.
The first dose of antibiotics should be administered STAT.
Consideration for ordering stress-dose hydrocortisone and STAT vasopressors drip may be made. If there is anticipation for a vasoactive infusion, a second vascular site needs to be established.
After the first hour, if the child shows a response to fluid administration (i.e., hemodynamics or normalized perfusion); ICU monitoring may be considered. However, if the child is not responsive to fluid, then therapy with vasoactive drugs should be initiated and titrated for the correction of poor perfusion or hypotension. Consideration of central and arterial venous access is warranted.
If the child is normotensive, having a normal BP, then therapy may begin with dopamine; norepinephrine may be considered if the child is hypotensive with vasodilated (warm) shock; norepinephrine may be replaced with epinephrine if the child is hypotensive with vasoconstricted (cold) shock.
Following vasoactive drug therapy, venous oximetry should be performed to check for central venous oxygen saturation (ScvO2). Generally, for warm shock, if the ScvO2 ≥ 70% with low BP, additional boluses of norepinephrine should be given with or without vasopressin. Generally, for cold shock, if ScvO2 < 70% with poor perfusion and low BP, a blood transfusion may be given (generally not indicated when the hemoglobin (hgb) concentration is above 10 g/dL) while optimizing arterial oxygen saturation. Additional boluses of fluid may be considered, either dobutamine along with norepinephrine or epinephrine alone may be considered.
Adrenal insufficiency is suspected if the child shows fluid-refractory shock. In such condition, baseline cortisol should be drawn and stimulation with adrenocorticotropic hormone (ACTH) should occur. Tests may be carried out if not sure of the steroid needs. Hydrocortisone (around 2 mg/kg bolus up to a maximum of 100 mg) may be given when adrenal insufficiency is suspected.
#4: Drugs used in PALS
#4: Drugs used in PALS
This algorithm outlines the doses and indications for the different drugs used in the treatment of children.
Adenosine: is generally indicated for supraventricular tachycardia (SVT). A first rapid push of 0.1 mg/kg IV/IO with a maximum of 6 mg should be given. This should be followed by a second rapid push of 0.2 mg/kg IV/IO up to a maximum of 12 mg.
Albumin: is indicated for trauma, shock, and burns. A rapid infusion of 0.5–1.0 g/kg IV/IO (10–20 mL/kg 5% solution) should be given.
Albuterol: is indicated for conditions of hypokalemia, asthma, and anaphylaxis (bronchospasm). It can be taken in various forms. When using a MDI (metered-dose inhaler), take 4–8 puffs through inhalation or as needed for 20 minutes with a spacer, if intubated via endotracheal intubation. When using a nebulizer for a child weighing less than 20 kg, 2.5 mg/dose and for child weighing greater than 20 kg, 5.0 mg/dose or use as needed for 20 minutes. When using a continuous nebulizer, via inhalation, 0.5 mg/kg per hour up to a maximum of 20 mg per hour.
Amiodarone: is used in ventricular tachycardia (VT) with pulses or when SVT rhythms are observed. It should be taken over a period of 20–60 minutes at 5 mg/kg IV/IO load up to a maximum of 300 mg. The medication may be repeated once daily at a maximum 15 mg/kg or 2.2 g in the adolescents. Amiodarone is also used in cases of pulseless arrest (i.e., pulseless Ventricular tachycardia (VT)/Ventricular Fibrillation (VF). It should be given as a bolus of 5 mg/kg IV/IO up to a maximum of 300 mg with similar kind of repetition dose as mentioned earlier.
Atropine sulfate: is indicated for symptomatic bradycardia. It should be taken as 0.02 mg/kg IV/IO with a minimum dose of 0.1 mg while the maximum doses are 0.5 mg and 1.0 mg for children and adolescents respectively while the repeat maximum dose should be 1 mg and 3 mg for children and adolescents. Via endotracheal (ET) route, the dose given should be 0.04–0.06 mg. Atropine sulfate is also used in drug overdose or toxin intake (i.e., organophosphate, carbamate, etc.). In a child less than 12 years of age, it should be initially given at 0.02–0.05 mg/kg IV/IO then IV/IO repeated for 20–30 minutes until the reversion of muscarinic symptoms. In a child greater than 12 years of age, the medication initially starts at 2 mg followed by 1–2 mg IV/IO for 20–30 minutes till the reversion of muscarinic symptoms.
Calcium chloride 10%: is indicated in hyperkalemia, hypocalcemia, overdose of calcium channel blocker, and hypermagnesemia. During arrest, the dose should be given as a slow push at 20 mg/kg (0.2 mL/kg) IV/IO and then repeated as needed.
Dexamethasone: is used during croup at 0.6 mg/kg PO/IM/IV up to a maximum dose of 16 mg.
Dextrose (glucose): is used in treating hypoglycemia and given at 0.5–1.0 g/kg IV/IO.
Diphenhydramine: is indicated for treating anaphylactic shock and given at a dose of 1–2 mg/kg IV/IO/IM over a period of 4–6 hours up to a maximum dose of 50 mg.
Dobutamine: is indicated in cardiogenic shock and congestive heart failure. It is used as an infusion of 2–20 mcg/kg per minute IV/IO and titrated to get the desired effect.
Dopamine: is used in cases of cardiogenic shock and distributive shock. It is used as an infusion of 2–20 mcg/kg per minute IV/IO and titrated to get the desired effect.
Epinephrine: is indicated in multiple conditions:
- It is used for the treatment of pulseless arrest and symptomatic bradycardia. Here, 0.01 mg/kg (0.1 mL/kg from a standard 1:10000 concentration) IV/IO for a period of 3–5 minutes up to a maximum single dose of 1 mg; when intubated, 0.1 mg/kg (0.1 mL/kg from a standard 1:1000 concentration) for a period of 3–5 minutes.
- While treating hypotensive shock, it is given as an infusion of 0.1 mcg/kg per minute IV/IO while considering higher dose if required.
- It is given in asthma subcutaneously at 0.01 mg/kg (0.01 mL/kg from stock concentration 1:1000) for 15 minutes with a maximum dose of 0.3 mg.
- For treating croup, it is used as inhalation at 0.25–0.50 mg of 2.25% racemic solution mixed with normal saline. 3 mL of epinephrine is mixed in 3 mL normal saline to get a 0.25 mL epinephrine racemic solution and used via inhalation.
- In anaphylaxis treatment in the case of children weighing less 30 kg, 0.3 mg is used via IM autoinjector and for children weighing between 10–30 kg, 0.15 mg is used via IM junior autoinjector. It is used at 0.01 mg/kg (0.01 ml/kg from a 1:1000 concentration) IV/IO for 15 minutes or as required with a single maximum dose of 0.3 mg.
- If the child is hypotensive then 0.01 mg/kg is used (0.1 mL/kg from 1:10000 standard concentration) IV/IO for 3–5 minutes with a maximum dose of 1 mg. If hypotension is found to persist despite the use of IM injection and fluid is then used as an infusion of 0.1–1.0 mcg/kg per minute IV/IO.
#5: Drugs used in PALS (continued)
#5: Drugs used in PALS (continued)
This algorithm outlines the doses and indications for the different drugs used in the treatment of children.
Etomidate: is indicated for the treatment of repetitive strain injury (RSI). It is used as an infusion of 0.2–0.4 mg/kg IV/IO over a period of 30–60 seconds with a maximum dose of 20 mg. This dosage is good enough to produce a sedative effect lasting 10–15 minutes.
Hydrocortisone: is indicated in adrenal insufficiency and is used as bolus of 2 mg/kg IV with a maximum dose of 100 mg.
Ipratropium bromide: is indicated in the treatment of asthma at a dose of 250–500 mcg through inhalation for 20 minutes or as needed up to 3 doses.
Lidocaine: is indicated in VF/pulseless VT and in wide complex tachycardia at a bolus of 1 mg/kg IV/IO. Maintenance should be an infusion of 20–50 mcg/kg IV/IO per minute; the bolus dose may be repeated if infusion is started after 15 minutes after the initial bolus. If intubated, dose should be 3–5 mg/kg ET.
Magnesium sulfate: is indicated in asthma (refractory status asthmaticus), hypomagnesemia, and torsades de pointes. For treating pulseless VT, a bolus dose of 25–50 mg/kg IV/IO up to a maximum dose of 2 g may be given; the treatment should be over 10–20 minutes for VT with pulses; and for treating asthma, it should be carried out with a slow infusion over 15–30 minutes.
Methylprednisolone: is indicated in asthma (status asthmaticus) and anaphylactic shock. The dose should be 2 mg/kg IV/IO/IM up to a maximum of 60 mg while methylprednisolone acetate should only be given IM; the maintenance is at 0.5 mg/kg IV/IO for 6 hours duration up to a maximum of 120 mg.
Milrinone: is indicated during increased SVR/PVR and myocardial dysfunction. The loading dose should be 50 mcg/kg IV/IO over 10–60 minutes, which may be followed by an infusion of 0.25–0.75 mcg/kg per minute IV/IO.
Naloxone: is used in the reversal of narcotic (opiate). For total reversal (i.e., secondary to overdose narcotic toxicity), subcutaneous bolus dose of 0.1 mg/kg IV/IO/IM is given for 2 minutes up to a maximum of 2 mg. If total reversal is not needed (i.e., therapeutic narcotic induced respiratory depression), subcutaneous dose of 1–5 mcg/kg IV/IO/IM is given and titrated to the desired effect. In order to maintain reversal, an infusion of 0.002–0.16 mg/kg per hour IV/IO is used.
Nitroglycerin: is indicated in cardiogenic shock and congestive heart failure. The drug is given as an infusion initially at 0.25–0.5 mcg/kg per minute IV/IO and as per tolerance titrated by 1 mcg/kg per minute for a period of 15–20 minutes. The usual dose range is 1–5 mcg/kg per minute with a maximum dose of 10 mcg/kg per minute. The dose should begin at 5–10 mcg per minute in adolescents with a maximum dose of 200 mcg per minute.
Nitroprusside: is indicated in severe hypertension and cardiogenic shock (associated with high SVR). The initial dose should be given at 0.3–1.0 mcg/kg per minute and titrated up as needed to 8 mcg/kg per minute.
Norepinephrine: is indicated in hypotensive shock (i.e., fluid refractory and low SVR) and used as an infusion of 0.1–2 mcg/kg per minute, titrated to the desired effect.
Procainamide: is indicated in VT (with pulses), SVT and atrial flutter; and given at a dose of 15 mg/kg IV/IO over 30–60 minutes. However, it should not be routinely used in combination with amiodarone.
Prostaglandin E1 (PGE1): is used in all forms of ductal-dependent congenital heart disease and given initially in an infusion of 0.05–0.1 mcg/kg per minute and then followed by 0.01–0.05 mcg/kg per minute IV/IO.
Sodium bicarbonate: is indicated in hyperkalemia and severe metabolic acidosis. It is administered as a slow bolus of 1 mEq/kg IV/IO; in the overdose of a sodium channel blocker (e.g., tricyclic antidepressant) a bolus dose of 1–2 mEq/kg IV/IO is used until the serum pH is greater than 7.45 (for cases of severe poisoning, it should be between 7.5–7.55). This is followed by an infusion of 150 mEq IV/IO NaHCO3/L solution and titrated for maintaining alkalosis.
Terbutaline: is indicated in hyperkalemia and asthma (status asthmaticus). An infusion dose of 0.1–10 mcg/kg per minute IV/IO while considering a bolus of 10 mcg/kg IV/IO over 5 minutes. Until IV/IO infusion is initiated, a subcutaneous dose of 10 mcg/kg for 10–15 minutes with a maximum dose of 0.4 mg.
Vasopressin: is indicated in cardiac arrest and catecholamine-resistant hypotension. In cardiac arrest a bolus dose of 0.4–1.0 unit/kg up to a maximum of 40 units is used; in catecholamine-resistant hypotension, continuous infusion of 0.0002–0.002 unit/kg per minute (0.2–2.0 milliunits/kg per minute) is given.
#11: PALS post-resuscitation care
#11: PALS post-resuscitation care
The PALS management of shock after ROSC algorithm outlines the steps of evaluation and care following cardiac arrest.
Depending on the patient’s hydration status and clinical condition, the composition and rate of intravenous fluid administration may be adjusted after the initial stabilization.
In case of infants, generally a continuous infusion of solution containing dextrose may be provided. For critically ill children, hypotonic solutions should be avoided. For all patients, isotonic solutions, such as lactated Ringer’s with or without dextrose or normal saline (0.9% NaCl), may be provided based on the child's clinical status.
Printed crash cart cards

Order the full set of printed crash cart cards.

Planning to certify/recertify ACLS?
Get a reminder when you need to take the exam
Please verify or enter a different email address:
How we reviewed this article
Our experts continually monitor the medical science space, and we update our articles when new information becomes available.
-
Current versionMail the author of this pageEmail
- Sep 22, 2024
-
Copy edited by:
Copy editorsChanges: Corrected compression parameters and medication dosing per AHA PALS - Jul 29, 2021
-
Written by: